Financial Mishaps in Budget Allocation for Capital Planning, Resulting in Fund Leakage and Potential Adversity for Patient Care
In the realm of healthcare, effective capital planning plays a crucial role in aligning resources with patient needs, improving operational workflows, and safeguarding long-term financial health. However, common mistakes can impair decision-making, inflate operational costs, and misalign capital investments with patient care priorities.
Mistakes in healthcare capital planning often stem from relying on siloed or outdated data, ignoring lifecycle costs of assets, under-budgeting for contingencies, lacking cross-functional visibility, failing to involve all critical stakeholders, neglecting risk assessments, and poor strategic alignment of projects with organizational goals.
To avoid these pitfalls, healthcare organizations can take several steps. First, adopting modern, integrated Capital Management and Maintenance Systems (CMMS) provides a dynamic dashboard consolidating live asset and budget data, creating a single source of truth and eliminating siloed information.
Second, incorporating full lifecycle cost and Total Cost of Ownership (TCO) analysis ensures that capital decisions reflect not just purchase price but future maintenance and replacement costs, preventing underestimation of long-term expenses.
Third, enabling cross-departmental collaboration by unifying maintenance, finance, and clinical stakeholders through shared data platforms and aligned priorities ensures that clinical safety and operational feasibility are fully considered.
Fourth, conducting rigorous risk and clinical feedback assessments on capital projects prioritizes assets by criticality and aligns with patient safety goals. This includes scenario planning to budget for unexpected contingencies like regulatory changes or failures.
Fifth, ensuring capital projects are strategically aligned with the hospital or healthcare system’s goals, regulatory frameworks, and reimbursement realities prevents disconnected investments that do not improve core service delivery or financial outcomes.
Sixth, applying accurate financial modeling and operational assumptions considers market dynamics, payer reimbursement shifts, and demographic changes, enabling ongoing validation and adjustment of project forecasts to maintain relevance and financial sustainability.
Seventh, maintaining clear documentation, training, and consistent application of accounting principles ensures that budgeting reflects actual expenses and revenues, avoiding distortions that can mislead capital planning decisions.
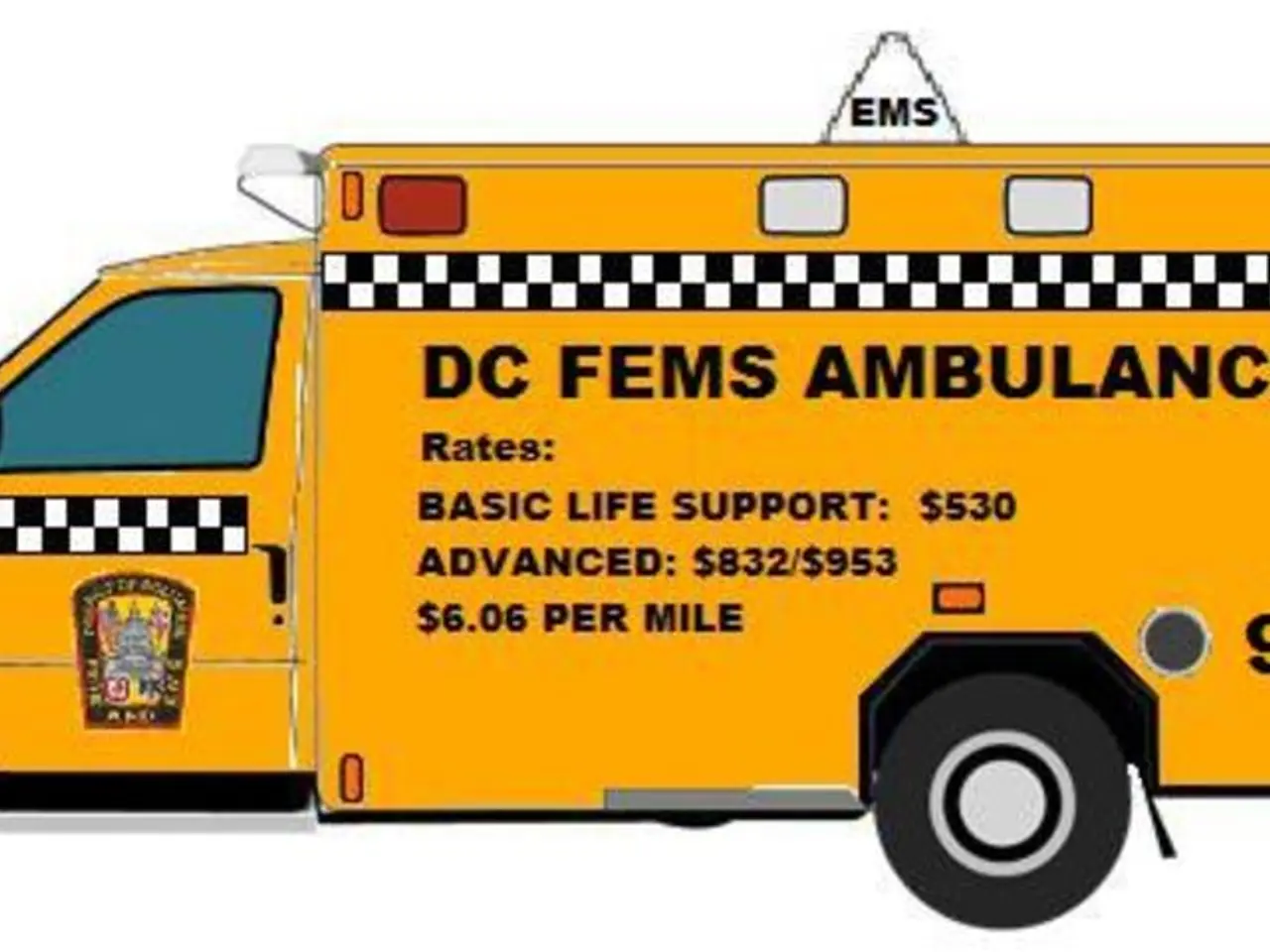
The financial impact of equipment downtime is significant, including lost revenue from canceled or rescheduled procedures, increased patient length of stay or transfers to other facilities, potential harm to patients due to delayed care, and reputational damage from service disruptions. Key questions to explore in capital planning include tracking equipment age and performance, having a validated, up-to-date inventory, involving clinical teams in purchasing decisions, assessing cybersecurity risks, leveraging standardization, and having visibility into purchasing across departments.
Missing the power of standardization in equipment purchasing can lead to higher service and training costs, missed volume discounts, and inefficiencies in procurement and support. Letting the loudest voices drive the budget can lead to inequity and missed opportunities to invest where it matters most. Outdated devices can be liabilities, lacking modern cybersecurity protections or the ability to integrate with electronic health records.
Capital planning in healthcare is a strategic process impacting patient care, operational efficiency, and financial sustainability. ECRI, a team of seasoned clinicians and biomedical engineers, offers predictive replacement planning services to help healthcare organizations build a smarter capital planning roadmap. Their Predictive Replacement Plan can help transform capital planning from a pain point into a strategic advantage by providing a clearer, data-driven view of capital needs, avoiding costly missteps, uncovering savings opportunities, and building a capital strategy that's fair, defensible, and ready for what's next.
Contacting ECRI can provide more information about their predictive replacement planning services and help healthcare organizations build a smarter capital planning roadmap. Overlooking the cost of underfunding critical but quieter departments can lead to skewed capital allocation that doesn't reflect priorities, resulting in delayed or denied access to essential equipment for patient care. The cost of doing nothing in capital planning can be operational, clinical, and reputational, with annual hospital budgeting mistakes costing health systems millions. Unplanned equipment purchases due to failures can lead to premium prices, lost revenue, and reputational damage. Overbuying technology that doesn't align with clinical needs can lead to underutilized assets, higher training and maintenance costs, and misallocated funds. Ignoring cybersecurity and integration risks can expose organizations to data breaches, compliance risks, and IT and clinical workflow disruptions. Capital planning that isn't tied to long-term organizational strategy risks misallocating resources and missing opportunities for growth, such as investments that don't support future care models, missed opportunities to support high-impact service lines, and fragmented planning that hinders transformation.
- In healthcare, effective capital planning ensures resources align with patient needs, improves workflows, and safeguards long-term financial health.
- Common mistakes in healthcare capital planning can impair decision-making, inflate operational costs, and misalign investments with patient care priorities.
- Adopting Capital Management and Maintenance Systems consolidates live asset and budget data, providing a single source of truth and eliminating siloed information.
- Full lifecycle cost analysis ensures capital decisions consider not just purchase price but future maintenance and replacement costs.
- Cross-departmental collaboration, involving all stakeholders and unifying maintenance, finance, and clinical teams, ensures clinical safety and operational feasibility are considered.
- Risk and clinical feedback assessments prioritize assets by criticality and align with patient safety goals, including scenario planning for contingencies.
- Aligning capital projects with an organization’s goals prevents disconnected investments that don't improve core service delivery or financial outcomes.
- Accurate financial modeling and operational assumptions consider market dynamics, payer reimbursement shifts, and demographic changes for ongoing project validation and adjustment.
- Consistent documentation, training, and accounting principles ensure budgeting reflects actual expenses and revenues, avoiding distortions that impact capital planning decisions.
- Healthcare organizations can benefit from ECRI's predictive replacement planning services, which provide a clearer, data-driven view of capital needs and help avoid costly missteps, uncover savings opportunities, and build a sustainable and strategic capital plan.